T
he Centers for Medicare & Medicaid Services (CMS) held an interesting and informative Section 111 reporting Town Hall call for workers’ compensation, liability, and no fault insurance claims payers and their agents and administrators. The call broke a bit of news, as it provided some updated guidance on a number of more advanced (yet common) Section 111 reporting issues.
The call featured a number of familiar representatives from both CMS and its Section 111 reporting contractor, the Benefits Coordination and Recovery Contractor (BCRC). The BCRC was once again represented by Angel Pagan, who began the call by emphasizing the importance of accurate Section 111 reporting. Here’s a recap of the important items addressed by CMS.
The Importance of Accurate Reporting
The presentation emphasized the continued importance of accurate Section 111 reporting. For the first time, CMS and the BCRC published statistics on the most common errors recently encountered by RREs. By far the most common error is invalid representative phone number, with more than 6,000 errors. This error is a “soft” error, meaning the file will still process but RREs are directed to correct the error anyway. Other “Top 10” errors included invalid TINs, invalid ICD codes, and invalid cause codes. The Top 10 recent errors can be found in this table supplied during the presentation:
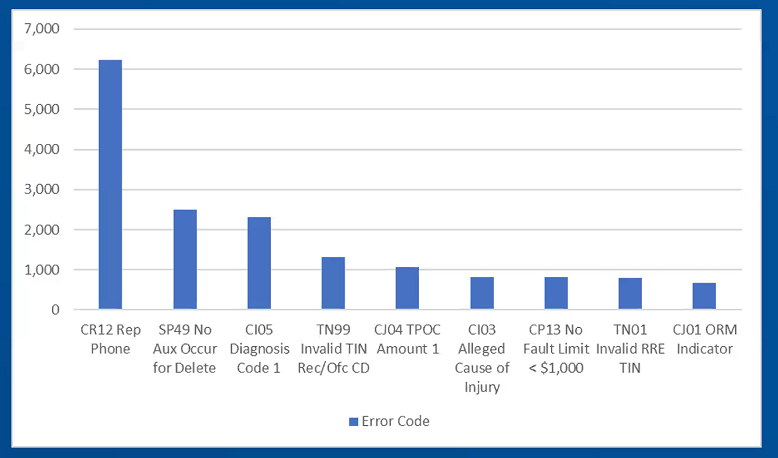
It is important to emphasize that ECS generally advises against reporting these optional fields that could create a soft-error and our MIR Service platform utilizes sophisticated business intelligence rules to prevent these types of errors from occurring.
Takeover Claims
For the first time, CMS and the BCRC outlined suggestions on what to do when claims move from one handling entity to another, such as from TPA-1 to TPA-2, or from a TPA to the RRE for self-handling, or vice versa. CMS and the BCRC suggested that when new claims are going to a TPA and existing claims will remain at an RRE or another TPA, then the RRE could simply acquire a new RRE. Where existing and new claims are moving from one TPA to another, CMS suggests a combination of delete and add records, where the old data is supplied via a delete record and the new data is supplied via an add record.
It is important to point out, however, that CMS and the BCRC assumed that the policy number changed when claims moved between TPAs or back to the RRE. The policy number is a key field and, if the policy number changes, then a “delete-add” combination is the only way to update the claim. In ECS’ experience, movement of claims between TPAs does not necessarily alter or adjust the policy number, but to the extent that it does, this CMS and BCRC announcement is the logical extension of a decision made within the last couple of years to make policy number a “key field.” There’s a lot to unpack about this particular topic, and we strongly encourage anyone with questions to reach out to their assigned ECS MMSEA Compliance Manager.
Recovery Issues
A number of questions were raised during the call about the impact of Section 111 reporting on conditional payment recovery demands. CMS and the BCRC emphasized the importance of accurate reporting of ICD codes as a means to reduce unwanted conditional payment demands, particularly avoiding reporting pre-existing or unrelated medical codes. CMS and the BCRC also reminded RREs that recovery agents can dispute conditional payment claims prior to demand without a written letter of authority, but after the demand stage a letter of authority from the debtor was required.
CMS and the BCRC will publish a transcript of the presentation as well as copies of the slides used within the next few weeks. In the meantime, should you have any questions about the presentation or what it means to your organization, contact your local ECS representative, Marty Cassavoy, or Scott Huber.
